Next-Generation Primary Care: How “Going to the Doctor” Is Changing
The future of healthcare is being driven by digital transformations and emerging technology that provide preventive, personalized and predictive medicine.
- By Amy Scanlin, MS
As the healthcare industry continues to suffer from provider shortages and increasing costs, the opportunity to rethink how patients receive care is leading to a collaborative and cohesive provider/patient approach. Supported by an acceleration in technological innovations, soon “going to the doctor” will encompass data as a decision-making tool like never before.
Today’s patients are seeking a proactive approach to their healthcare journey. As wearables and software as service devices are providing increasingly complex information and suggesting clear linkages between choices, genetics and their direct impacts on health quality and longevity, interest in biometric feedback is gaining speed.
The expectation in today’s connected world is for providers to be able to use patient-generated data and make informed decisions from it. The challenge for many providers, however, is the amount and speed in which data pours into the healthcare system, limiting an ability to use it to its fullest potential. By current estimates, 97 percent of data in hospitals already goes unused,1 and the exponential growth of medical knowledge continues to double every 72 days.2 This immense overload of information, coupled with the challenge of parsing out which data is most beneficial for the creation of a personalized care approach, can place roadblocks between providers and patients.
In some cases, data overload is prompting calls for specializations within healthcare fields that include data architecture and analysis that support subspecializations to aggressively target patients’ specific disease states.
To that end, research and development funding in support of enhanced digital tools for the benefit of preventive, personalized and predictive medicine is increasing, as is support for AI-supported decision-making, diagnostics and specialty medicine programs. All of this data requires an analytical assessment to most effectively interpret and provide meaningful information that providers can use in determining patient care.
Artificial Intelligence in Healthcare
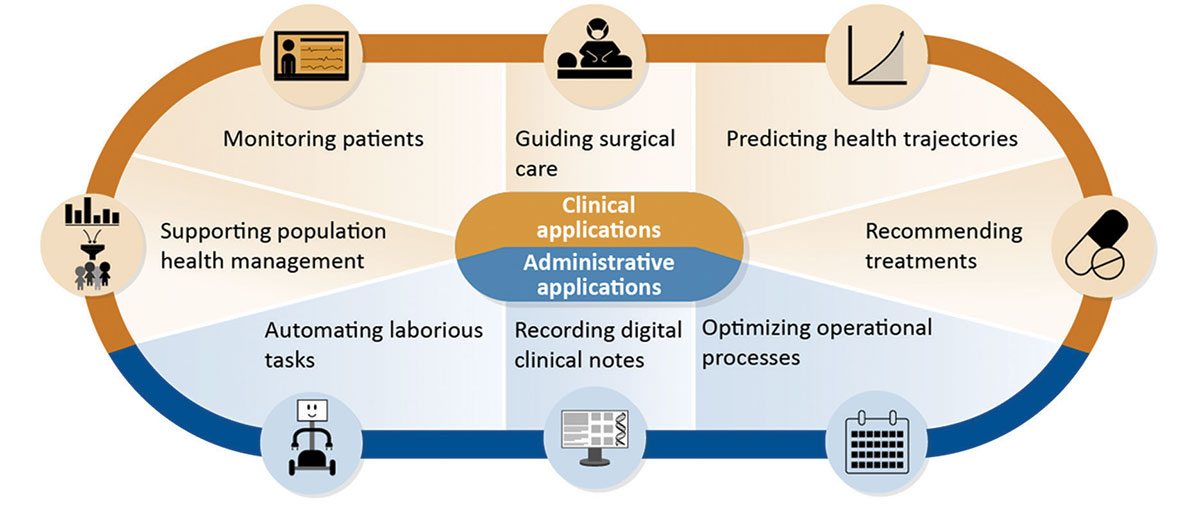
Source: Artificial Intelligence in Health Care: Benefits and Challenges of Technnologies to Augment Patient Care. U.S. Government Accountability Office, Nov. 30, 2020. Accessed at www.gao.gov/products/gao-21-7sp.
Productivity
In an industry in which an increasing patient load is leading to reduced time spent with each individual, AI tools, when properly integrated and interconnected, may be able to offer a solution to an overscheduled, overburdened workforce. Automating routine paperwork, billing, insurance and scheduling are some key areas where AI-enabled tools are already offering time-saving assistance. AI is also being studied and strengthened to support decision-making. Even newer AI technologies, known as ambient intelligence, are coming into the marketplace. Ambient intelligence listens and transcribes patient-provider conversations so that it can analyze the type of visit, input that information into electronic medical records (EMRs) and assign CPT billing codes. Providers need never turn away from their patients to add notes into an EMR.2
Smart technologies are helping to improve the healthcare experience for both patients and clinicians. Patients appreciate that smart technologies allow their provider to better focus on their needs, and physicians may find use of AI means less time required for administrative duties. Work-life balance is a significant frustration for healthcare professionals as cited in a GE HealthCare study titled “Reimagining Better Health,”3 and the administrative duties related to patient care is one such cause prompting some clinicians to leave the industry. If things do not improve, there may be a projected 12.9 million worldwide shortage of healthcare professionals by 2035.4
Though touted by some and distrusted by others, AI language learning models are here to stay and will continue to improve. By 2030, use of AI natural language processing is not only expected to be widespread, but predictive analytics is expected to be functional by 2035.5
Proactivity
Today’s connected patients are interested in and well-informed about their healthcare risks, using data to inform behaviors as they take greater control of their healthcare journey. This proactive interest is leading to a greater emphasis on design of preventive care plans tailored to patients’ needs as opposed to treating conditions once they arise.
In the current healthcare model that favors treatment over prevention, 80 percent of health dollars are spent on 20 percent of patients. This trend is expected to continue with expenditures reaching $7 trillion by 2030 and $11.8 trillion by 2040. However, at the same time, expenditures on health promotion services are also expected to grow to approximately $8.3 trillion by 2040.6 Spending on wellness devices and software apps, in particular, is growing as interest in innovation, accelerated technologies, data interoperability, architecture and analysis is helping to positively influence disease prevention by reducing health risks and delaying disease onset thanks to earlier diagnoses.
By some estimates, 16 percent of global consumers surveyed own a wearable device that tracks or monitors their health, and in the U.S., 14 percent of those surveyed had been prescribed a mobile health app by a healthcare provider. With an interest in health technologies comes an opportunity for providers to help patients understand the data their devices provide and to make informed choices based on this data. And while data delivered by mobile devices rarely makes its way into patients’ EMRs today, it can still be integrated into traditional healthcare.5
Greater Specialization
As the pace of research and available data grow, some have questioned whether there is too much new healthcare information for generalists to stay on top of. Aging baby boomers (almost one-third of the world’s population will be 65 and older by 2025),5 companion diagnostics, personalized care and an ever-increasing detailed knowledge of every known and emerging health condition are prompting the need for specialized care with subspecialty groups emerging.
Although consumers are collecting and using data specific to their own health, the prevalence of chronic conditions and our understanding of them continues to grow. Some specializations are specific to diagnoses, treatment and care management. Still other specializations focus on how to set up and use AI technologies to benefit healthcare systems and workplaces. Subspecialties are laser focused on the intricacies of specific diseases or treatments, and how to parse big data to generate personalized, meaningful data. As AI technologies continue to evolve, being able to identify pertinent information from it will evolve, too, causing data to become more broad but also more laser-focused. Medical specialists and subspecialists will rely on data specialists to support their analysis and decision-making tools for the benefit of patients.
Using Data to Support Telehealth Systems
Virtual care is a familiar solution that continues to ease scheduling burdens while improving access to care. As technology advances and remote monitoring of portable data becomes better integrated with standard healthcare metrics, consumers may one day be able to bypass routine telehealth appointments in favor of addressing many of their own healthcare needs at home.
In some cases, providers assign patients responsibility for monitoring their own “always-on” health data and basic diagnostic testing so they can report updates through patient portals. In other cases, wearables report this data directly back to healthcare providers or software as service providers with data directly ported into patients’ EMRs. Virtual real-time monitoring and reporting is helping to improve patient outcomes since it can eliminate or reduce the costs required for routine office visits.
Combining virtual and in-person care is another approach that is easing bedside staffing burdens. For example, in-person physical examinations remain a cornerstone of patient care, but administrative tasks such as discharge paperwork, care instructions and follow-up appointment scheduling can be handled by a remote provider.”7
The Way Ahead
Providers should think about preparing for a future of connected and integrated healthcare by taking a hard look at their current capability gaps and budgeting needs to fill them. Examples include replacing outdated software to capture always-on patient data, improving high-speed connectivity and developing staff and patient buy-in of new systems that include training on how to use them most effectively. Hesitation in a new and disruptive digital world can be eased by thoughtfully approaching the problem. Think about what kind of data should be collected and how it will be used and secured. Include whether new data and analytics specialties will need to be brought online to analyze and interpret.
Maintaining a personal connection between providers and patients is imperative, particularly in a digital, virtual world. In fact, strengthening these relationship practices and bringing digital tools online may be more critical to long-term success than ever. Equally important to communicating how to use these new technologies is why they have been incorporated into the care environment and how they will benefit the processes currently in place.
Consider new technology plans, particularly from patients’ points of view with a special eye toward those who may be technology disadvantaged. Some, hopefully most, patients will be excited by the updates and enthusiastic for the increased participation and collaboration in their own care. But others may feel confusion and frustration, particularly those who value human interaction over technology.
Special attention must be given during any transitions to ensure no patients, regardless of their interest in and aptitude for technology, feel left behind. While digital technology is certainly not expected to replace in-person care, patients who are engaged in a digital future could replace their providers if they do not integrate into the digital world.8 Even so, these tech-inclined patients are not the only individuals who must be considered.
In the rapidly changing healthcare industry, fueled in large part by digital transformations and emerging technology, the evolving healthcare model is likely to look quite different from today’s. Use of wearables and analysis of patient data generated from them are driving a future of precision patient care and enabling rapid interventions for the benefit of all.6
References
1. Six Trends That Are Shaping the Future of Healthcare. GE Healthcare, July 13, 2023. Accessed at www.gehealthcare.com/insights/article/six-trends-that-are-shaping-the-future-of-healthcare.
2. The Future of AI in Medicine and What It Means for Physicians and Practices with Tom Lawry. JAMA Network, July 25, 2023. Accessed at www.ama-assn.org/practice-management/digital/future-ai-medicine-and-what-it-means-physicians-and-practices-tom-lawry.
3. GE Healthcare Study: Reimagining Better Health. Accessed at www.gehealthcare.com/insights/reimagining-better-health.
4. PWC Health Research Institute. Global Top Health Industry Issues: Defining the Healthcare of the Future. Accessed at www.pwc.com/gx/en/healthcare/pdf/global-top-health-industry-issues-2018-pwc.pdf.
5. Fernandes, L, FitzPatrick, M, and Roycroft, M. The Role of the Future Physician: Building on Shifting Sands. Clinical Medicine, May 20, 2020. Accessed at www.ncbi.nlm.nih.gov/pmc/articles/PMC7354041.
6. Deloitte. Navigating the Future of Health™ in an Era of Change. Accessed at www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/future-of-health.html.
7. McCarthy, A. Transforming Virtual Care Models. Harvard Medical School Trends in Medicine, May 29, 2024. Accessed at postgraduateeducation.hms.harvard.edu/trends-medicine/transforming-virtual-care-models.
8. James, TA. How Physicians Can Prepare for the Future of Healthcare. Harvard Medical School Trends in Medicine, May 14, 2021. Accessed at postgraduateeducation.hms.harvard.edu/trends-medicine/how-physicians-can-prepare-future-health-care.