Myths and Facts: Autoimmune Disorders
Until more is discovered about the causes of autoimmune disorders, these chronic but sometimes fatal disorders will continue to increase in numbers of diseases and individuals affected.
- By Ronale Tucker Rhodes, MS
JUST A DECADE or two ago, most people had likely never heard of an autoimmune disorder (AD). But, today, the growing number of individuals diagnosed with an AD is alarming. The National Institutes of Health (NIH) estimates more than 23 million Americans live with an AD, whereas the American Autoimmune Related Diseases Association (AARDA) says that number is 50 million.1,2 To put this in perspective, the AD prevalence equals heart disease and cancer combined.3
What’s more, each year, it appears the incidence rate of ADs is increasing. According to Geoff Rutledge, MD, PhD, a California-based physician and chief medical officer at HealthTap (a technology company delivering a suite of connected health apps), “A recent review of literature concluded that worldwide rates of rheumatic, endocrinological, gastrointestinal and neurological autoimmune disorders are increasing by 4 to 7 percent per year, with the greatest increases seen in celiac disease, type 1 diabetes and myasthenia gravis, and the greatest increases occurring in countries in the Northern and Western Hemispheres.”1 In addition, the American Diabetes Association found type 1 diabetes alone increased by 23 percent between 2001 and 2009.4
In the 1940s, autoimmunity was a fairly new concept, with little evidence to support it as a cause of pathology.5 Then, in the 1950s, Henry G. Kunkel, MD, known as the father of immunopathology, began studying patients with rheumatoid arthritis and lupus in The Rockefeller Hospital. Using newly developed tools of protein chemistry, Dr. Kunkel and colleagues demonstrated that certain antibodies in the blood of these patients reacted with other antibodies as if they were antigens. This was later coined the “rheumatoid factor,” which is now used as a test to measure the amount of proteins produced by the immune system that can attack healthy tissue in the body, which can help to pinpoint an AD diagnosis.6,7
ADs affect women at a rate of about two to one compared with men (6.4 percent of women vs. 2.7 percent of men), and the disease often starts during their childbearing years (ages 14 through 44). Some ADs are more common in certain ethnic groups. For instance, lupus affects more African-American and Hispanic people than Caucasians. And, certain ADs such as multiple sclerosis and lupus run in families with a susceptibility.8
Yet, while it is not definitively understood what causes AD, researchers suspect environmental factors like infections and exposures to chemicals and solvents are interfering with the immune system’s ability to distinguish self from nonself. Indeed, it is universally agreed by scientists that most of the risk of autoimmunity comes from environmental exposures rather than from genetic susceptibilities.8,9 In addition, the Western diet is suspected as a trigger because it is high in fat, sugar and processed foods that cause inflammation. Another theory is the hygiene hypothesis, which suggests that because kids aren’t exposed to as many germs today, their immune system may overreact to harmless substances.8 And, for women specifically, some clinical scientists suspect estrogen may be the culprit, causing a woman’s immune system to produce more antibodies and increasing the likelihood that her body will turn on itself.10
What is certain about ADs is their effects on an increasing number of people and how much remains unknown about them, which is likely the reason many myths and misconceptions surround ADs.
Separating Myth from Fact
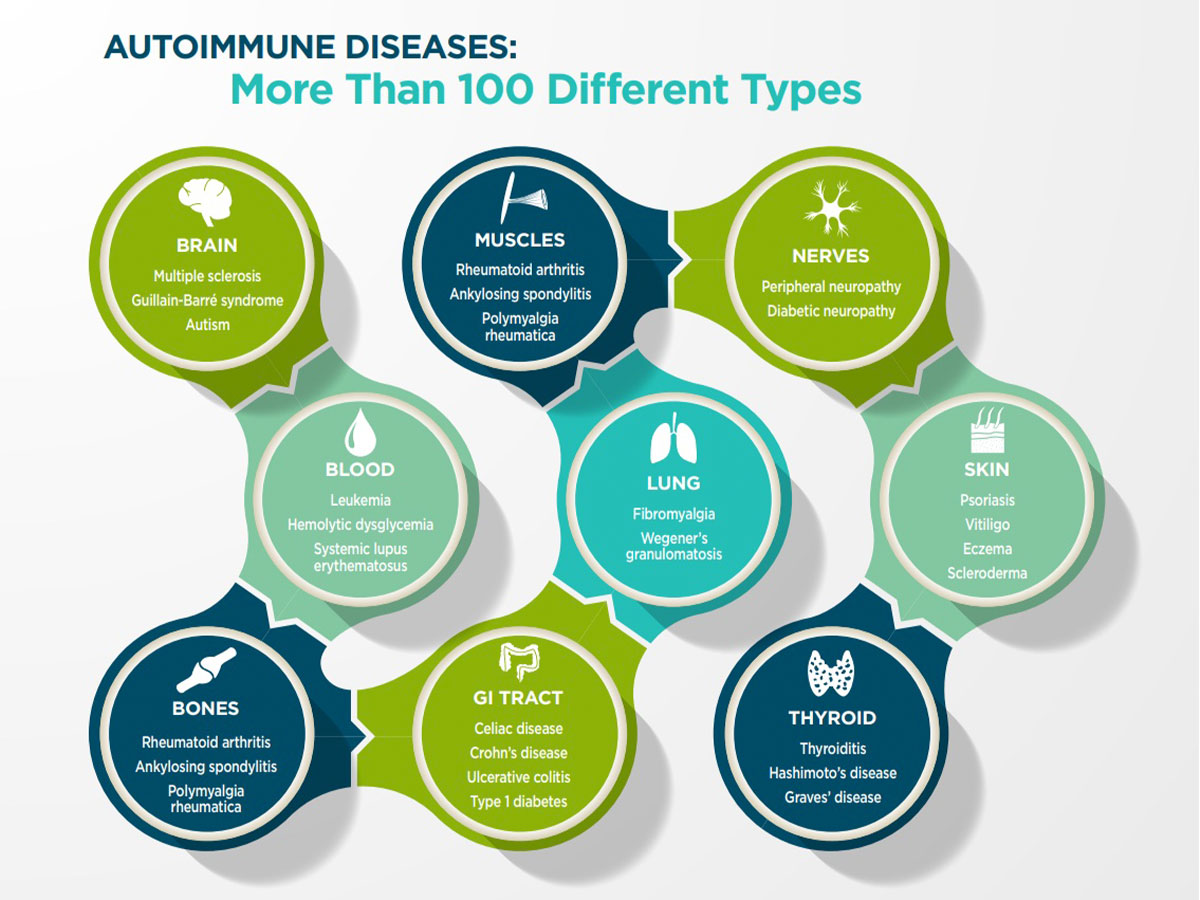
Myth: There are not that many types of ADs.
Fact: While the jury is out on how many ADs there are in the U.S, there are a lot of ADs that have been identified, and it is predicted many more diseases could have an autoimmune basis. The NIH report that stated 23.5 million Americans are living with AD mentions 80 different diseases, but it bases that number on another report that refers to only 24 diseases, as well as potential misdiagnosis and underdiagnosis and the possibility more ADs might be discovered. The AARDA website states the number of Americans living with AD is 50 million based on its determination that more diseases could be autoimmune. Indeed, AARDA states researchers have identified 80 to 100 different ADs and suspect at least 40 more of having an autoimmune basis.11
The Autoimmune Registry (ARI), a 501(c)3 nonprofit corporation founded in 2016 to create a hub for research, statistics and patient data on all autoimmune illnesses, is working with four academic medical centers to examine their electronic medical records to determine how many people suffer from the diseases believed to be caused by autoimmunity. While ARI acknowledges it will not be able to account for misdiagnosis and underdiagnosis since not all diseases have medical codes and medical codes are often wrong, its goal is to develop statistics reasonably consistent for the U.S. population.11
Myth: If someone looks well, he or she can’t be suffering from an AD.
Fact: Many ADs are invisible, so individuals’ appearance doesn’t necessarily reflect their health or how they feel. Unlike most diagnosed cancer patients who look sick (especially under treatment), most AD patients look superficially well, even while suffering significant morbidity, lost productivity and debilitating financial stress.3
Myth: Younger people can’t get ADs, and symptoms of AD in older adults are just a result of age.
Fact: The age at which people can be affected by an AD depends on the disorder/disease. While women are more likely to be diagnosed with an AD during childbearing years, ADs can affect people of any age. There’s no such thing as being too young, and the effects of the disease as one ages are different from the natural aging process.12 Indeed, ADs tend to arise early in life. For instance, type 1 diabetes starts in childhood or adolescence, and rheumatoid arthritis and systemic lupus erythematosus (SLE) start during the 20s and 30s. However, these conditions often worsen and lead to complications later in life when they become more noticeable, which is why ADs are often thought to more likely affect the elderly.13
A 12-year study of irritable bowel disease (IBD), one of the most common ADs that affects about 1.2 million Americans, found the incidence rate in children doubled between 1991 and 2002. 3 Other very common ADs in children include liver disease, celiac disease, Addison’s disease, autoimmune thyroiditis, juvenile arthritis, juvenile scleroderma, type 1 diabetes, Kawasaki’s disease, multiple autoimmune syndrome and pediatric lupus.14 In adults, the most common ADs include type 1 diabetes, rheumatoid arthritis, psoriasis, multiple sclerosis, lupus, IBD, Crohn’s disease, ulcerative colitis, Addison’s disease, Graves’ disease, Sjogren’s syndrome, Hashimoto’s thyroiditis, myasthenia gravis, vasculitis, pernicious anemia and celiac disease.15
Myth: People with ADs experience the same symptoms.
Fact: Symptoms of AD depend on the disease pathology. There are two types of ADs: systemic and localized. Systemic ADs tend to spread to various organs, from the skin to the kidneys, as well as the heart. Localized ADs have an effect on a particular body organ like the thyroid, liver or adrenal glands. ADs can have an effect on any body part since they can affect joints, blood vessels, red blood cells, connective tissues, muscles or even endocrine glands (such as the pancreas or thyroid).14
General symptoms of AD have the maximum probability of emerging in the very beginning, whereas other unique abnormalities might appear later. In adults, each AD has its own peculiar set of symptoms, yet many share similar features such as muscle aches, joint pain, signs of inflammation (redness, heat or pain) and flu-like symptoms. Fatigue is a defining symptom of many ADs.16 In children, the first very common symptoms are dizziness, slight fever, fatigue, dry mouth or eyes, weight loss, diffuse joint pain and skin rashes.14
Myth: ADs are contagious.
Fact: At this time, experts do not believe ADs are spread to others like bacterial or viral infections. For instance, ADs caused by white blood cells contracted through shared needles, blood transfusion or organ transplant aren’t contagious possibly because the number of white blood cells transferred by these methods is relatively small. While researchers have been able to transfer some ADs in mice by transferring certain white blood cells, this only occurs when the mice are already immune-deficient specially bred mice that are already prone to AD. Organ transplants are also unlikely to transfer AD, again presumably because the amount of white blood cells is still relatively small, and the person’s normal immune system handles it (even though transplant patients are immunocompromised).17
The only known transfer of autoimmunity occurs between mother and fetus during pregnancy, and that is still rare even in affected mothers. For example, mothers with lupus can give birth to babies with neonatal lupus; similarly, myasthenia gravis can cause neonatal myasthenia gravis.17
Interestingly, though, one study points to a higher risk of developing a nonceliac AD by spouses of people who have celiac disease in which a person’s immune system attacks the lining of their small intestines when gluten-containing foods are eaten. This connection indicates potentially some sort of shared environment, or even gut bacteria, is the culprit. The study’s authors also suggest the connection could be the result of something called ascertainment bias, where a spouse of someone with celiac disease is more likely to seek medical advice about similar symptoms.18
Myth: ADs are easy to diagnose.
Fact: ADs consist of a host of diseases, many of which are very rare, widely scattered over a number of medical specialties, and usually grouped by body system (digestive, joints, metabolic) rather than as a category with common causal mechanisms (immune system attacks own tissues). That’s why diagnosis and treatment are a notoriously exhausting journey, with patients seeing on average five doctors over three and a half years before receiving a diagnosis.4
Furthermore, diagnosis can be tricky. This is because symptoms often come and go, which makes it difficult to pinpoint the problem unless the physician happens to know the individual has a family history of AD. In many cases, it’s necessary to follow a patient for a while so the disease will manifest itself.16
As mentioned earlier, a rheumatoid factor test is one blood test primarily used to help pinpoint a diagnosis. A positive rheumatoid factor test result indicates a high level of rheumatoid factor was detected in the blood, which is associated with AD. 19 But, it’s important to know that blood tests that look for autoantibodies can yield positive results even when someone doesn’t have an AD.16 For instance, a number of other diseases and conditions can raise rheumatoid factor levels, including cancer, chronic infections, inflammatory lung diseases, mixed connective tissue disease, Sjögren’s syndrome and SLE. In addition, some healthy people (particularly older adults) have positive rheumatoid factor tests, although it’s not understood why. Even some people who have rheumatoid arthritis (one of the most common forms of AD in adults) have low levels of rheumatoid factor.19
Other blood tests used to pinpoint a diagnosis include the anti-nuclear antibody, anti-cyclic citrullinated peptide antibodies, C-reactive protein and erythrocyte sedimentation rate tests.19
Myth: ADs can be cured.
Fact: Despite the growing number of ADs, scientists are still in the dark regarding interventions that can help cure them. While some may resolve, usually spontaneously and for unknown reasons, most do not. But, ADs can go into remission with therapy. The main goal of therapy is to suppress disease flares and extend periods of remission, if remission is attainable.20
Treatment for ADs include medication, physical therapy, exercise, nutrition and, for some, complementary and alternative medicine (CAM). Medications prescribed depend on the disease, its severity and symptoms. These include nonsteroidal anti-inflammatory drugs such as ibuprofen and aspirin to relieve mild symptoms; prescription drugs to relieve more severe symptoms such as pain, swelling, depression, anxiety, sleep problems, fatigue or rashes; medicines that replace vital substances the body no longer makes such as insulin, hormones and enzymes; corticosteroids to decrease inflammation and reduce the activity of the immune system; biologics (immune-suppressing drugs) to control inflammation and help control disease process and preserve organ function; plasmapheresis to remove antibodies from the bloodstream, thereby preventing them from attacking their targets; and immune globulin (protein replacement therapy).21,22
When an AD affects joints, muscles and bones, physical therapy can help to reinforce muscles and help individuals move body parts more easily. Eating a well-balanced diet and getting regular exercise can also help individuals feel better. In addition, physicians may suggest supplements to replace insulin, hormones or vitamins.14
While it’s hard to know if CAM therapies will work for ADs, some people do opt to try them. Some examples of CAM therapies include herbal products, chiropractic, acupuncture and hypnosis. However, there are limited studies on these therapies, and it’s important for patients to discuss them with physicians since some products can cause health problems or interfere with medicines.22
Myth: ADs are not life-threatening.
Fact: With an estimated 100-plus ADs today, most are usually chronic and not fatal; however, some can lead to death. In fact, ADs are one of the 10 leading causes of death for girls and women in all age groups (up to 64 years old).2 The most common ADs that can cause death include Graves’ disease, giant cell myocarditis, Addison’s disease, granulomatosis with polyangiitis and SLE.13,23
Dispelling the Myths Now
While ADs were barely even heard of until the last couple of decades, they are growing in both numbers of diseases and individuals affected. Thankfully, the novel approach to thestudy of immunology by Dr. Kunkel, who discovered autoimmunity, has vastly expanded our knowledge of how immune cells work and how they can go awry.5 Now, more is understood about these mostly chronic but sometimes fatal disorders, but much remains to be learned.
In 2003, NIH released its Autoimmune Diseases Research Plan encouraging research into the causes, treatments and prevention of AD, with the goal of obtaining additional funding. Since then, the National Institute of Allergy and Infectious Diseases has made it a priority to study ADs because “the chronic and debilitating nature of these diseases, which can lead to high medical costs and reduced quality of life, is a burden on patients and also affects their families and communities.”24 Indeed, based on data from the last decade, estimates of the total AD financial burden are around $100 billion.3 It can only be hoped, then, that continued study will improve outcomes for the millions of people affected by ADs.
References
- Travers C. Why Autoimmune Diseases Are on the Rise. Shape, Dec. 13, 2016. Accessed at www.shape.com/ lifestyle/mind-and-body/why-autoimmune-diseases-are-rise.
- Ribeiro M. 10 Facts and Statistics About Autoimmune Diseases. Scleroderma News, Oct. 30, 2017. Accessed at sclerodermanews.com/2017/10/30/autoimmune-facts-statistics.
- Feldman B. An Invisible Epidemic—When Your Body Attacks Itself—Autoimmune Disease. Accessed at tincture.io/an-invisible-epidemic-when-your-body-attacks-itself-autoimmune-disease-5738b699de12.
- Rattue G. Autoimmune Disease Rates Increasing. Medical News Today, June 22, 2012. Accessed at www.medicalnewstoday.com/articles/246960.php.
- The Rockefeller University. Henry G. Kunkel. Accessed atwww.rockefeller.edu/our-scientists/2284-henry-g-kunkel.
- The Rockefeller University. The Discovery of Autoimmune Diseases. Accessed at centennial.rucares.org/ index.php?page=Autoimmune_Diseases.
- Mayo Clinic, Rheumatoid Factor. Accessed at www.mayoclinic.org/tests-procedures/rheumatoid-factor/ about/pac-20384800.
- Watson S. Autoimmune Diseases: Types, Symptoms, Causes and More. Healthline, Oct. 18, 2017. Accessed at www.healthline.com/health/autoimmune-disorders#causes.
- Kerr D. Foreword to The Autoimmune Epidemic by Donna Jackson Nakazawa. Touchstone, February 2009. Accessed at donnajacksonnakazawa.com/the-autoimmune-epidemic-excerpt.
- Harper R. When Your Body Attacks: The Important Facts About Autoimmune Diseases. Accessed at www.ruthieharper.com/when-your-body-attacks.
- Autoimmune Registry. Estimates of Prevalence for Autoimmune Disease. Accessed at www.autoimmune registry.org/autoimmune-statistics.
- Wyant P. Myths About AutoimmuneDiseaseThat MakeIt Even Harderto Live With.The Mighty, June 28, 2018. Accessed at themighty.com/2018/06/autoimmune-disease-myths-misconceptions.
- 10 Facts About Autoimmune Diseases. Accessed at www.healthhype.com/10-facts-about-autoimmune-diseases.html.
- Sen A. Autoimmune Diseases In Children — Symptoms & Treatment. Boldsky, Jan. 27, 2017. Accessed at www.boldsky.com/pregnancy-parenting/kids/2017/autoimmune-diseases-in-children-110469.htm.
- Healthline. Autoimmune Diseases: Types, Symptoms, Causes and More. Accessed at www.healthline.com/health/autoimmune-disorders.
- 9 Autoimmune Diseases Every Woman Needs to Know About. Accessed at www.health.com/lupus/ autoimmune-diseases?
- Right Diagnosis. Is Autoimmune Disease Contagious? Accessed at www.rightdiagnosis.com/a/ai/contagious.htm.
- Shomon M. Causes of Autoimmune Diseases. VeryWell.com, Aug. 31, 2018. Accessed at www.verywellhealth.com/what-are-the-causes-of-autoimmune-diseases-3232655.
- Mayo Clinic. Rheumatoid Factor. Accessed at www.mayoclinic.org/tests-procedures/rheumatoidfactor/about/pac-20384800.
- McCain J. The Disease Burden of the Most Common Autoimmune Diseases. Managed Care, July 19, 2016. Accessed at www.managedcaremag.com/archives/2016/7/disease-burden-most-common-autoimmune-diseases.
- Right Diagnosis. Treatments for Autoimmune Diseases. Accessed at www.rightdiagnosis.com/a/ai/treatments.htm.
- Office on Women’s Health. Autoimmune Diseases. Accessed at www.womenshealth.gov/a-z-topics/autoimmune-diseases.
- Drain K. The 4 Deadliest Autoimmune Disorders: Signs You Need To Know. Medical Daily, Feb. 21, 2017. Accessed at www.medicaldaily.com/4-deadliest-autoimmune-disorders-signs-you-need-know-411716.
- National Institute of Allergy and Infectious Disease. Autoimmune Diseases. Accessed at www.niaid.nih.gov/ diseases-conditions/autoimmune-diseases.
