Meeting the Demand for Personalized Care
As a patient-driven priority, personalized healthcare is poised to become a permanent fixture in the public health landscape.
- By Trudie Mitschang
THE CONCEPT OF healthcare consumerism is not new, but it has definitely evolved. As healthcare costs continue to rise, patients are looking for healthcare experiences that mirror those they have in other service sectors, with an increasing expectation that interactions with providers and payers be as frictionless as those in the hospitality, airline or e-commerce industries.
Armed with an arsenal of Internet-based research, today’s patients are technologically savvy and personally empowered to expect a higher caliber of care that factors in their unique health profiles and lifestyles. No longer content to passively accept treatment plans, this new-breed patient expects and even demands solutions that cater to their needs and preferences. They also want care that is backed by data — not just physician opinions.
One recent survey conducted by Abbott found that while 79 percent of patients have confidence in physicians’ decision-making ability, they believe technology is needed to deliver more personalized care.1 Another survey by Accenture found that 88 percent of healthcare consumers expect their care to be as personalized as their experiences during online shopping or vacation planning. The survey identified four essential components that define human-centric, personalized healthcare, including the need for empathetic emotional support, ease of access to care through technology, a desire for increased trust in the physician/patient relationship and an emphasis on equitable care.2
In a 2022 Healthcare Insights Study conducted by CVS Health, 1,000 U.S. consumers and 400 healthcare providers were asked what kind of healthcare experience they would like and what kinds of barriers hinder their ability to receive optimal health outcomes. The survey stated, “Providers and consumers agree that increasing engagement and communication improves health outcomes. Whether their goal is decreasing daily stress levels or increasing overall wellbeing, 81 percent of consumers say it is very important their primary care provider is “aware of their overall happiness and life satisfaction levels and aware of how they deal with difficult emotions and stress.”3
Additional highlights from the CVS survey include:
- Ninety-two percent of consumer respondents said that convenience is an important factor when choosing a primary care provider; 33 percent of those respondents scheduled a virtual visit to save money and/or time.
- Fifty-three percent of healthcare provider respondents said that adding virtual care options resulted in more visits.
- The majority of healthcare provider respondents — 94 percent — said that interventions such as text message reminders or phone follow-ups assist patients in following their prescribed care plan.
Genomics as a Key Driver of Personalized Care
Genomic medicine, which involves understanding how a person’s genetic makeup influences their health, has become a cornerstone of personalized care. With the Human Genome Project’s completion in 2003 and subsequent breakthroughs in genomic-based research, healthcare providers can now analyze a patient’s genetic information to predict, diagnose and treat diseases more precisely and personally than ever.4
“The Holy Grail in healthcare has long been personalized medicine, or what is now called precision medicine,” says Kemal Malik, member of the Bayer board of management responsible for innovation. “But getting to the level of precision we wanted wasn’t possible until now. What’s changed is our ability to sequence the human genome.”4
Many diseases, including cancers, are caused by alterations in our genes. Genomics can detect a disease long before symptoms present themselves, allowing for early diagnosis and more successful treatment outcomes. For instance, genetic testing for BRCA1 and BRCA2 mutations has become common in assessing breast cancer risk, allowing for proactive measures in prevention and early detection.
“Healthcare will move more toward prevention rather than cure,” Malik says. “To date, genomics has had the most impact on cancer, because we can get tissue, sequence it and identify the alterations.” In the United States, the Cancer Genome Atlas has mapped the key genomic changes in more than 30 types of cancer. Such databases could deliver a definitive diagnosis in seconds, and even recommend targeted treatments based on the DNA of both the patient and the disease.4
The Human Genome Project has fueled the discovery of nearly 2,000 disease genes, and these are proving highly effective at providing fast and accurate analysis. As genomics and biotechnology continue to evolve, the demand for tailored treatments is expected to rise as well.
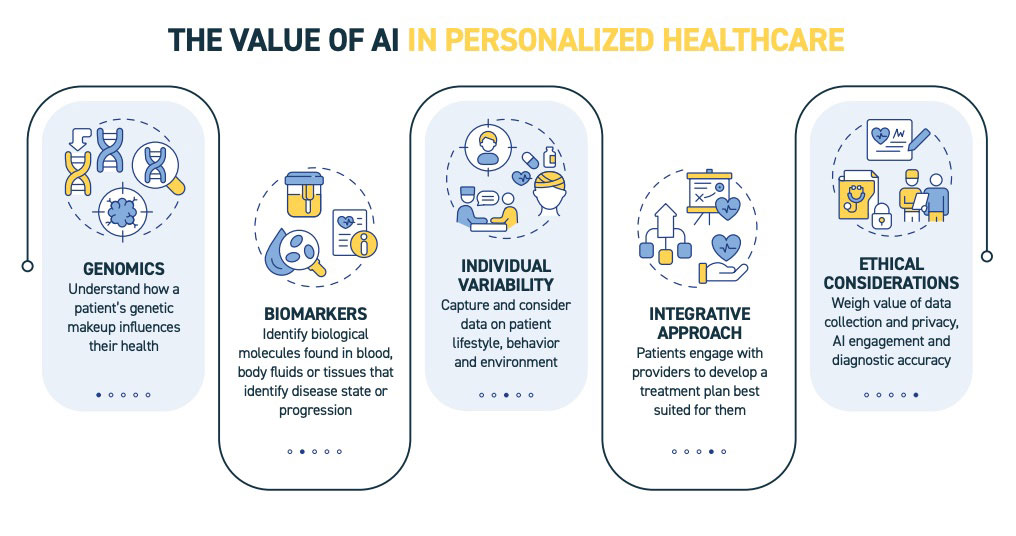
The Influence of AI
The integration of artificial intelligence (AI) and machine learning into healthcare has also enhanced personalized care by enabling data analysis on a large scale. AI can process vast amounts of patient data and provide recommendations based on patterns that human clinicians might not easily recognize.
In the clinical setting, particularly in oncology, AI tools have the potential to personalize diagnosis and treatment for patients by drawing on a variety of data types, from genomics and electronic health records to environmental factors.
AI algorithms fall into three broad categories: machine learning, language processing and computer vision. Among them, computer vision has been one of the fastest-moving areas of AI development. In recent years, a multitude of new programs and commercial partnerships have cropped up around algorithms that read images, such as radiology scans or histology slides, and detect markers indicative of disease presence or progression with equal or greater precision than human experts.5
For example, digital pathology firm PathAI boasts a long list of biotech and pharma partnerships, including one with Roche Tissue Diagnostics to develop AI-driven companion diagnostics for identifying subsets of patients most likely to benefit from various treatments. Other companies developing AI-based digital pathology tools for precision medicine include firms such as Paige and Tempus.5
In 2021, Paige became the first company to have an AI-based cancer diagnostic tool approved by the U.S. Food and Drug Administration. The tool, Paige Prostate, analyzes biopsied prostate tissue and identifies areas likely to contain cancer cells, which a human pathologist evaluates and confirms.
“When you’re talking about precision medicine, it’s about sub-segmenting the population into strata and trying to find the solutions that work for those specific segments of populations,” says Nimita Limaye, research vice president with IDC Health Insights.6
AI can be used to diagnose diseases, develop personalized treatment plans and assist clinicians with decision-making. Rather than simply automating tasks, AI is about developing technologies that can enhance patient care across healthcare settings. However, challenges related to data privacy, bias and the need for human expertise must be addressed for the responsible and effective implementation of AI in healthcare.
Precision Care for Chronic Disease
As chronic conditions such as diabetes, hypertension and obesity continue to rise globally, there is increasing recognition for the need to pursue personalized care plans. Since chronic diseases often require ongoing, complex management strategies that vary from patient to patient, personalized care approaches, including tailored dietary recommendations, medication regimens and lifestyle changes, have been shown to significantly improve patient outcomes.
One example is in the treatment of type 2 diabetes. Genetic research has identified several gene variants that influence the risk of developing this disease along with a patient’s response to specific drugs, such as metformin, a common treatment for managing blood glucose levels. According to a study in Diabetes Care, a variant of the SLC2A2 gene affects how efficiently the body absorbs glucose from the blood. Understanding this variation helps doctors select the most effective drug and dosage for individuals with specific genetic profiles.7
Cardiovascular disease, including conditions such as hypertension, coronary artery disease and heart failure, is another area where precision medicine is making an impact. Onesize-fits-all treatment approaches may not always provide the best outcomes due to variations in how patients respond to medications such as statins or anticoagulants. Through genetic testing, precision medicine can identify patients with specific genetic variants that may influence their risk of adverse effects from statins (used to lower cholesterol) or help determine which patients will benefit most from anticoagulant therapies to prevent strokes or heart attacks. A well-known example is the CYP2C19 gene, which affects how patients metabolize clopidogrel, a blood thinner used to prevent blood clots in people with heart disease. Individuals with certain variants of this gene are less likely to benefit from clopidogrel, and precision medicine can help guide alternative treatment strategies.8
Asthma, a chronic respiratory condition characterized by airway inflammation and breathing difficulties, affects individuals differently, with some experiencing mild symptoms and others dealing with severe, life-threatening episodes. Precision medicine has revealed that asthma is not a single disease but a collection of subtypes, each with different underlying mechanisms. One of the key breakthroughs in asthma management has been the identification of specific biomarkers that allow for targeted therapies. For example, patients with high levels of a specific inflammatory marker, known as eosinophils, may benefit from biologic therapies, such as monoclonal antibodies targeting interleukin-5 (IL-5), which reduces the number of eosinophils and helps control severe asthma symptoms. Treatments such as mepolizumab and benralizumab are more effective for patients with eosinophilic asthma than traditional inhaled corticosteroids, which are often the default treatment plan.9
Implications for Healthcare Providers and Systems
The growing demand for personalized care presents both opportunities and challenges for healthcare providers and systems. On the positive side, personalized care has the potential to improve patient outcomes, reduce hospital readmissions and enhance the overall patient experience. Patients receiving care tailored to their unique characteristics are more likely to adhere to treatment plans, leading to better health outcomes and cost savings in the long run.
A report from Harvard Business Review Analytic Services, an independent commercial research unit within Harvard Business Review, analyzed how expanding precision medicine offers healthcare providers new opportunities to provide high-value care and concluded that the expansion of precision medicine could have a major impact on outcomes and costs.10
“While precision medicine can be seen by some people as genomics-guided treatment, I think this definition is too limiting,” says Larry Chu, MD, MS, a Stanford professor who advised President Barack Obama on the 2015 Precision Medicine Initiative. “I think precision medicine means precisely diagnosing conditions, then integrating all relevant patient data and insights to guide care to the best outcomes. It is about providing the right treatment to the right patient at the right time.”10
The report argued that the practice of precision medicine will grow, thanks to the promise of benefits to healthcare organizations, providers and patients in the form of better outcomes and reduced costs. Research suggests that eliminating unwarranted variations in medical care can reduce the cost of patient management by at least 35 percent.10
However, the implementation of personalized care requires significant investments in technology, data management and clinician training. Healthcare providers must be able to access and analyze large amounts of patient data, including genetic information, to deliver personalized treatments. This requires advanced infrastructure and robust datasharing mechanisms to ensure patient information is securely stored and shared across different healthcare providers.
In addition, personalized care raises ethical concerns related to data privacy and equity in access. As healthcare becomes more tailored to individual needs, it is crucial to ensure all patients, regardless of socioeconomic status, have access to these advanced care models. Addressing these concerns will be essential for ensuring the equitable and effective delivery of personalized care.
The Road Ahead
Advances in genomics, patient expectations, technological innovation and the need for more effective chronic disease management all factor into the rising demand for personalized medicine. As healthcare systems continue to evolve, personalized care promises a more patientcentered experience. However, realizing the full potential of this trend will require a commitment to clinician training, investments in systems and technology integration and big-picture thinking when it comes to ensuring equitable access for all patient populations.
References
1. New Research Finds Physicians and Patients Point to Emerging Technology and Data as Central to Closing Treatment Gaps and Improving Vascular Health.Abbott press release, Aug. 19, 2020. Accessed at abbott.mediaroom.com/2020-08-19-New-ResearchFinds-Physicians-and-Patients-Point-to-Emerging-Technologyand-Data-as-Central-to-Closing-Treatment-Gaps-and-ImprovingVascular-Health.
2. Henderson, S. TheUltimateHealthcare Experience: Global Report. Accenture, Jan. 25, 2022. Accessed at www.accenture.com/us-en/insights/health/ultimate-healthcare-experience.
3. Wilder, J. Survey: Consumers Desire a More Personalized Healthcare Experience. Healthcare Innovation, July 13, 2022. Accessed at www.hcinnovationgroup.com/population-healthmanagement/consumerism/news/21273993/survey-consumersdesire-a-more-personalized-healthcare-experience.
4. Heggie, J. Genomics: A Revolution in Health Care? National Geographic, Feb. 20, 2019. Accessed at www.nationalgeographic.com/science/article/partner-content-genomics-health-care.
5. Shaffer, C. AI Could Reshape Precision Medicine, But First, Doctors Have to Trust It. Precision MedicineOnline, May 30, 2024. Accessed at www.precisionmedicineonline.com/precision-oncology/ai-could-reshape-precision-medicine-first-doctors-have-trust-it.
6. Horowitz, B. How Technology Integration Supports Precision Medicine. HealthTech, Feb. 10, 2023. Accessed at healthtechmagazine.net/article/2023/02/how-technologyintegration-supports-precision-medicine.
7. Henriques, M. Metformin Works Better for Some Diabetics Because of Gene Variant, Study Finds. Diabetes News Journal, Aug. 30, 2016. Accessed at diabetesnewsjournal.com/2016/08/30/metformin-works-better-for-some-diabeticsbecause-of-gene-variant-study-finds.
8. Anderson, CD, Biffi, A, Greenberg, SM, et al. Personalized Approaches to Clopidogrel Therapy: Are We There Yet? Stroke, 2010 Dec;41(12.1):2997-3002. Accessed at www.ahajournals.org/doi/10.1161/STROKEAHA.110.594069.
9. Rogers, L, Jesenak, M, Bjermer, L, et al. Biologics in Severe Asthma: A Pragmatic Approach for Choosing the Right Treatment for the Right Patient. Respiratory Medicine, 2023;218:107414. Accessed at www.resmedjournal.com/article/S0954-6111(23)00302-5/fulltext.
10. Precision Medicine Could Have a Major Impact on Healthcare Outcomes and Costs. Harvard Business Review, Dec. 7, 2018. Accessed at hbr.org/sponsored/2018/12/precision-medicinecould-have-a-major-impact-on-healthcare-outcomes-and-costs?